Other publications
The pace of technologic change: Implications for digital health behavior intervention research
Understanding and promoting effective engagement with digital behavior change interventions
Which self-regulation behaviour change techniques work in an alcohol reduction app? – – – Randomised control trial
How to build an alcohol reduction app – – – PhD thesis
The behavior change techniques used in alcohol reduction apps – – – Content analysis
What users think might increase usability in an alcohol reduction app – – – Think aloud and interview studies
Do digital interventions for alcohol reduction workin general? – – – Cochrane review
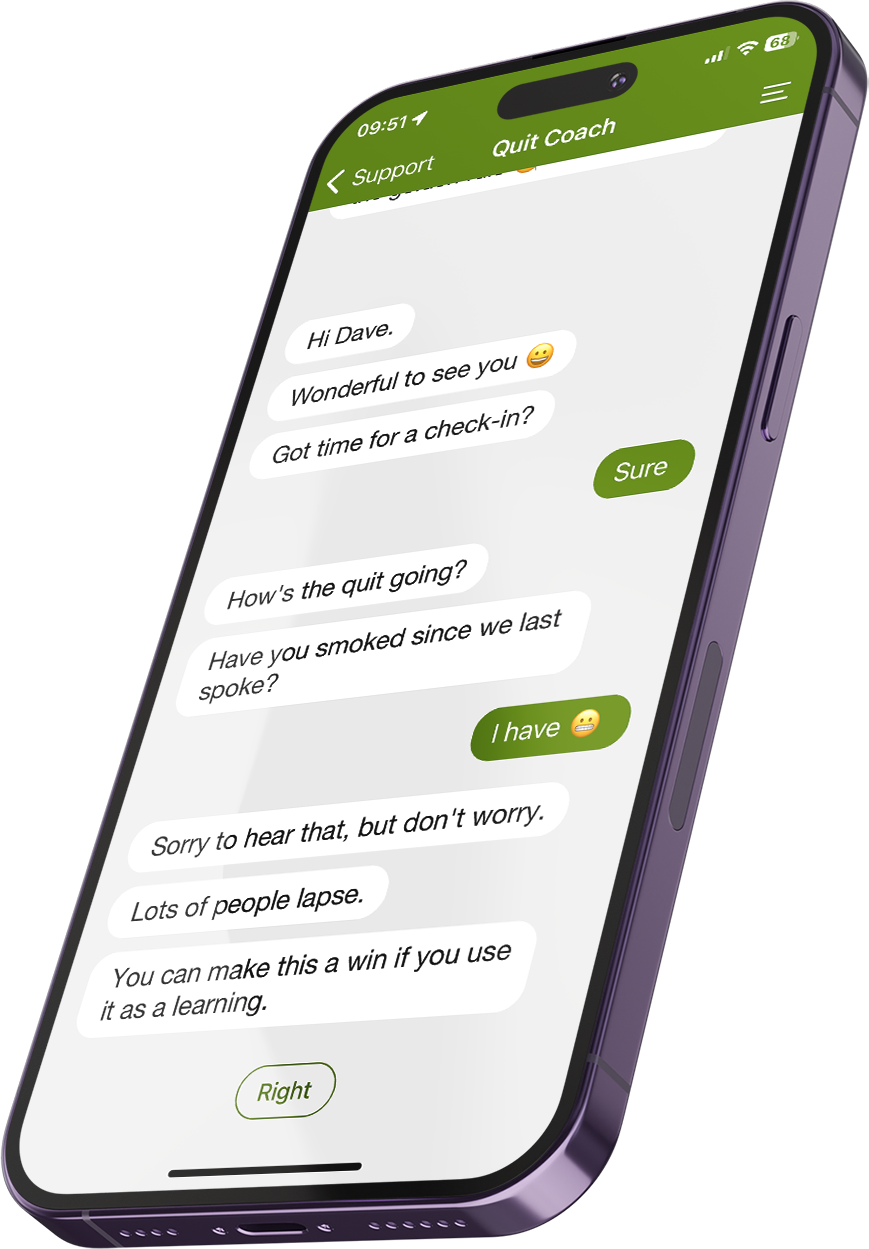
How an app for pregnant smokers was built – – – Process study
How to identify what behaviour change techniques should be included in an alcohol reduction app – – – Delphi study
Which behaviour change techniques are used in digital alcohol interventions – – – Meta-regression